For much of recent history, men have tended to die earlier than women, though this was not always the case: for many centuries, the perils of childbirth effectively nullified any advantage women had over men. But modern medical care has dramatically reduced maternal death, and women in most countries now have a consistent advantage in life expectancy compared with men.
According to the most recent US data, the average American man dies five years before the average American women, and even wider gaps are seen among different racial and ethnic minorities: for example, Asian American women live 16.5 years longer than African American men on average.
While disparities in life expectancy between men and women have typically been greeted with a collective shrug, these questions are taking on greater urgency as new research reveals ominous trends for men’s health. Researchers from Stanford demonstrate that in societies where maternal mortality from childbirth has improved and birth control reduces family size, women consistently outlive men.
In addition, the gap in life expectancy continues to widen with increasing income inequality. Although the gap in life expectancy had started to narrow in the 1970s, the overall death rate is again climbing, particularly for white American men, making it essential to understand why the state of men’s health is going from bad to worse.
Many people assume that shorter male lifespans are driven, directly or indirectly, by genetics and other biological factors. Yet a closer look at science, medicine, and culture suggests that the engine for this disparity might be the long-held ideal of masculinity itself. It is becoming increasingly clear that a “man’s man” might be the most dangerous thing a man can be.
Fundamental biology may indeed play a role in disparities in life expectancy, and many theories have explored this possibility. The higher rate of male births has been suggested as one reason for differences in survival, as has the need for better female health to ensure successful child-rearing.
The additional X chromosome carried by women might provide “backup” in the event of some genetic abnormalities. Higher levels of estrogen in women protect the heart from disease, and higher heart rates in women could simulate the beneficial effects of exercise.
On the other hand, increased risk-taking is associated with higher levels of testosterone in men. Males, too, show greater susceptibility for infections. These are just some of the hypotheses that have been advanced to explain differences in lifespan.
However, wide variation in life expectancy suggests that it is the behaviors and attitudes associated with gender, rather than the biological differences associated with sex, which are responsible for men dying sooner than women. For instance, the gender gap in lifespan favors women by 11.6 years in Russia, but approaches zero not only in some poor countries such as Mali but also in some high-income regions such as Santa Clara, California.
Furthermore, a study published earlier this year found no significant difference in the proportion of elderly trans men and non-trans men in the US, implying that behaviors stereotypically associated with male gender might explain why men are more likely to die younger than women.
Male behaviors and attitudes that affect their health – including notions about when it’s OK to seek help – are not fixed byproducts of genes and hormones, but are strongly influenced by culture. A traditional masculine ideal common in the US holds that “the most powerful men among men are those for whom health and safety are irrelevant.”
These ideals, a fatal concoction of risky behavior, anti-intellectualism, and unwillingness to seek help are reinforced by portrayals of masculinity in popular culture that emphasize “toughness, self-reliance, and stoicism” while tending to erase images of male aging and infirmity.
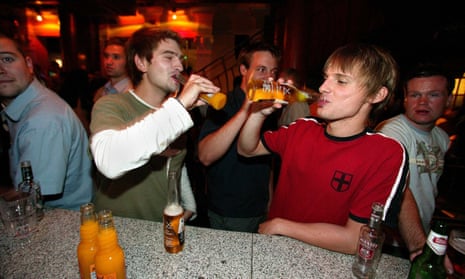
This traditional view of male identity comes with serious health consequences. Men are more likely to smoke and drink than women and therefore are more likely to suffer from health problems related to these behaviors. Importantly, not only are men less likely to see a doctor, they are also much less likely to seek psychological help. This is one of the main reasons why suicide rates, both intentional and unintentional from drug overdoses, remain much higher for men than women, and continue to rise.
While men are much less likely to attempt suicide, they are unfortunately much more likely to succeed when they do so, because of their preference for firearms. These issues are only becoming more urgent as the economic dislocations created by the transition to a knowledge-based economy continue to place additional stresses on US culture and communities.
It seems paradoxical that a segment of the US population that has historically enjoyed greater power and privilege can also be considered vulnerable. But unexamined assumptions about biological determinism, compounded by cultural ideas about masculinity, have created a situation that places men at risk for worse health outcomes from a surprisingly early age.
The internalization of a male identity in which seeking help is seen as a sign of weakness begins in childhood and becomes particularly intense during adolescence.
This maladaptation is reflected in widening gender gaps in educational achievement, with girls outperforming boys not only in the United States, but around the world. These gaps persist throughout the educational experience, leading to concerns that boys are not being prepared for success in the modern economy.
At the same time, however, studies show that what men consider “manly” varies by culture, and therefore might be modifiable. When researchers interviewed white patients who had survived a heart attack, they concluded that their “fears of being seen to be weak contributed to delays in seeking medical care and led to reluctance to disclose symptoms to others.”
Yet the same study found that south Asian men “emphasized wisdom, education and responsibility for the family and their own health as more valued masculine attributes, and this contributed to a greater willingness to seek medical help”.
To help close the gap in lifespans between the sexes, a public health campaign with support from the private sector is needed to help reshape what it means for men to seek medical and psychological help.
This might take the form of educational interventions, starting at an early age, that offer an idea of maleness in which seeking help from others is seen as a positive attribute, as well as increased mindfulness of the potential harmfulness of language and images that valorize self-destructive “masculine” behavior.
All of these considerations should occur within a research enterprise that addresses the gender survival chasm as a multifactorial issue that includes biological, psychological and psychobiological issues.
To ensure that our fathers, brothers, sons and friends stop dying prematurely, we need to fundamentally rethink what being a “man” is all about.