
If you live in a city, each room of your house has its own distinct broth of microbes splattered all over its walls—most of it from your skin, mouth, and gut. But if you live in a rural area, this broth contains a lot more microbes from the environment outside. Now, scientists in the burgeoning field of "microbial biogeography" say this could help us understand why people in cities tend to develop diseases that are very different from people in the country.
Your body is full of microbes—indeed, a recent estimate suggests there are more single-celled aliens in your body than there are human cells. The average human male has about 30 trillion cells and 40 trillion microbes living inside him. But these little invaders don't stop at the envelope of your flesh. They're constantly being sloughed off with your skin, dribbling out of your mouth, and getting pooped out of your colon. Which is where microbial biogeography comes in. It's the study of all the microbes that live in our environments, whether they come from us, other animals, or elsewhere in the natural world. Taken together, the microbes in an environment—whether it's your gut or the forest floor—are called a microbiome.
There have already been efforts to sequence microbiomes in people's homes, in the soils and waters of many different environments, and (memorably) on the New York City subway. From these experiments, we've learned that our environments are crawling with different kinds of microbes, many of which co-evolved with us and contribute to our good health. Now a new study conducted in and around Brazil reveals that the microbiomes in our homes change dramatically from country to city, and even from room to room in urban homes.
Can I swab your walls, please?
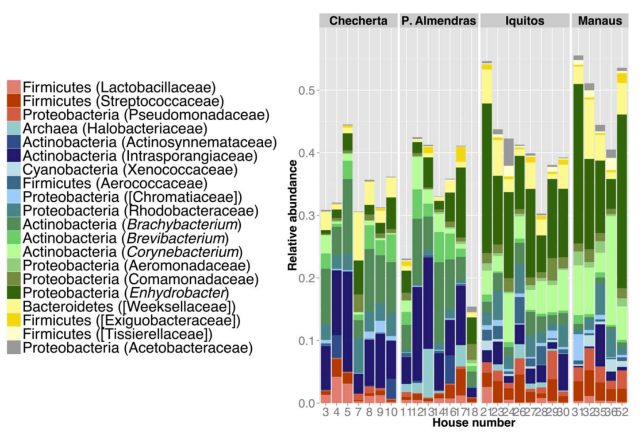
To conduct this experiment, a group of researchers picked four different human communities. In a paper published about their work today in Science Advances, they write:We measured community demographics and architectural parameters, and characterized the microbial communities of 10 houses and their inhabitants from each of four locations: [Checherta], a traditional jungle village of hunter-gatherers near the border between Peru and Ecuador, [Puerto Almendras], a rural village further east along a similar latitude, the large Peruvian town of Iquitos, and, finally, the modern Brazilian city of Manaus.
Checherta and Puerto Almendras have between 21 to 25 homes with extended families living in them, while Iquitos has 400,000 residents and Manaus has about 1.8 million. The researchers painstakingly used curettes to swab the floors and walls in each home, creating careful architectural maps showing the location where each sample was taken. Then they sequenced the DNA in the samples to identify the microbes.

Once they had identified a representative sample of the microbes in these homes, it quickly became clear that there was a definite pattern. People in Checherta and Puerto Almendras were living with a lot more microbes from the environment in their homes. But people in Iquitos and Manaus were living in baths of microbes that mostly came from humans.
In the town and city homes, researchers even found that they could identify rooms based on the microbes they found on the walls. Bathrooms were splashed with microbes that live in people's mouths, while kitchens harbored microbes that are commonly found in water.
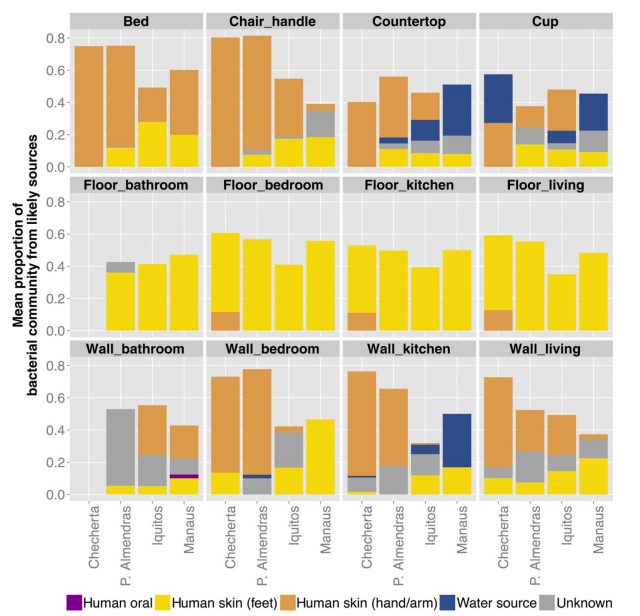
Other rooms were coated in microbes from the skin on human arms, while floors were blanketed with skin cells from feet. Walls apparently form microbial barriers, creating distinctive microbiomes. In the rural villages, homes had fewer walls—as a result, the microbial populations weren't as distinct.
Bioscientist Jack Gilbert, an Argonne National Lab researcher not involved with this study, told Ars that a key finding was that air exchange changed dramatically between rural and city homes:
When we look at air exchanges between our modern homes and homes for people living in economically-poor rural communities we often see that their homes have many orders of magnitude more air exchange with outside 'fresh' air than our modern homes—which makes sense, because such a constant exchange requires a lack of walls or any thermal or humidity regulation.
There are dramatic and often invisible differences between rural homes and urban homes, ranging from architectural features to how many microbes can get inside just from riding on the breeze.
Is my house making me sick?
One of the obvious questions that arises is whether the dramatic difference between rural and urban microbiomes has an impact on human health. Is it healthier to live in a home with more microbes from the natural environment?
Write the researchers:
These remarkable changes in house microbial content across urbanization might translate into differences in microbial exposure that may have developmental health implications for humans, according to several related hypotheses [the “hygiene” hypothesis, the “Old Friends” hypothesis, and the “Disappearing microbiota” hypothesis], suggesting that the reduced pattern of microbial exposure leads to immune and metabolic disorders that have become the new disease paradigm in the industrialized world.
These "related hypotheses" suggest that urban diseases like asthma may come from lack of exposure to the kinds of environmental microbes that the residents of Checherta encounter every day, in their homes. If we co-evolved with these microbes, and they have lived inside us for tens of thousands of years, maybe our bodies are suffering now that they are gone. This isn't just idle speculation: a great deal of medical research now is focused on how the microbes in our guts prevent cancer, regulate mood, and boost our immune systems.
MIT epidemiological researcher Ilana Brito, who was not involved in the study, told Ars that there is evidence to suggest that urban microbiomes may be a culprit in some ailments:
There's epidemiology work showing that exposure to farm animals and pets decreases asthma while exposure to urban allergens such as dust mites may promote asthma. The next crucial step will be to find out if any of these organisms are also linked with increased disease prevalence in rural or urban environments.
While it's tempting to say the solution is just to live a more rural lifestyle, Gilbert cautioned that the situation is more complex than that. Disease environments are created by social context as well as environment:
The types of diseases that people will be more or less susceptible to are likely to be influenced more by their socioeconomic background and access to medical care. So the individuals living in the airy-rural homes may have a reduced susceptibility to immune-regulation disease (allergies, asthma, etc), and maybe to other disease states associated with microbial dysregulation or dysbiosis—but they are also more likely to have not been vaccinated against common diseases, to not have access to modern healthcare, which will likely reduce their life-span.
In other words, country life and city life lead to different biogeographies, and therefore different health risks. Added Gilbert, "The question should not be, which is healthier, but which aspects of each home could be appropriated to improve health for all." We may not be able to change the microbiomes in our homes, but we can study them to figure out which medical problems they're likely to cause.
City doctors of the future may offer personalized medicine that's tailored to people's home environments to prevent common diseases of urban life.
Science Advances, 2016. DOI: 10.1126/sciadv.1501061
Listing image by Darin
reader comments
46